THESE ARE SOME IMAGES OF KINESIOLOGY TAPING THAT i HAVE DONE ALREADY
KINESIOLOGY TAPING:
I completed a 2 day course in the National School for Remedial Therapy in Dublin on Kinesiology Taping. I am now a qualified Kinesiology Taping Specialist and below is a list of injuries that can be treated using the Kinesiology Taping method of treatment. I com. Kinesiology Tape is applied to the injured muscle.
Reviews from people who have used Kinesiology Taping to treat their injuriesKt Tape Pro Review
"http://sportsmedinfo.net - KT Tape Pro exceeds the performance of all previous brands and versions. This new pro synthetic tape sticks through thick and thin... "
Total Views: 8,329 | Length: | Published: 01/22/2012 | Ave. Rating: 3.35 from 17 ratings
Pro-tec Athletics Kinesiology Taping: Plantar Fasciitis Review
"Former NFL trainer Jim Whitesel demonstrates the use of Pro-Tec Athletics' Kinesiology Tape to alleviate conditions of plantar fasciitis. "
Total Views: 20,462 | Length: 2:45 | Published: 12/12/2011 | Ave. Rating: 4.63 from 22 ratings
THE BENEFITS OF KINESIOLOGY TAPING
- Stabalises the injured areas without Restricting Movement
- Helps Prevent further injury
- Helps to re-educate the neuromuscular system
- Increases blood flow to the injured areas
- Can enhance performance
- Helps reduce pain and swelling
- Allows injured athlete to remain active
- Psychological benefits as well as the placebo effect
Injuries that can benefit from this type of treatment
 - PLANTER FASCIITIS
- PLANTER FASCIITIS
Plantar fasciitis also known as Plantar Heel Pain (PHP) is a painful inflammatory process of the plantar fascia, the connective tissue or ligament on the sole of the foot. It is often caused by overuse of the plantar fascia, increases in activities, weight or age. It is a very common condition and can be difficult to treat if not looked after properly. Longstanding cases of plantar fasciitis often demonstrate more degenerative changes than inflammatory changes, in which case they are termedplantar fasciosis. The suffix "osis" implies a pathology of chronic degeneration without inflammatory.
DIAGNOSIS: The diagnosis of plantar fasciitis is usually made by clinical examination alone. The clinical examination may include checking the patient’s feet and watching the patient stand and walk. The clinical examination will take under consideration a patient's medical history, physical activity, foot pain symptoms and more. The doctor may decide to use imaging studies like X-ray, diagnostic ultrasound and MRI.
Heel bone with heel spur An incidental finding associated with this condition is a jheel spur, a small bony calcification on the calcans heel bone, in which case it is the underlying plantar fasciitis that produces the pain, and not the spur itself. The condition is responsible for the creation of the spur; the plantar fasciitis is not caused by the spur. Sometimes ball-of-foot pain is mistakenly assumed to be derived from plantar fasciitis. A dull pain or numbness in the metatarsal region of the foot could instead be metatarsalgia, also called capsulitis. Some current studies suggest that plantar fasciitis is not actually inflamed plantar fascia, but merely an inflamed flexor digitorum brevis muscle (FDB) belly. Ultrasound evidence illustrates fluid within the FDB muscle belly, not the plantar fascia.
DIAGNOSIS: The diagnosis of plantar fasciitis is usually made by clinical examination alone. The clinical examination may include checking the patient’s feet and watching the patient stand and walk. The clinical examination will take under consideration a patient's medical history, physical activity, foot pain symptoms and more. The doctor may decide to use imaging studies like X-ray, diagnostic ultrasound and MRI.
Heel bone with heel spur An incidental finding associated with this condition is a jheel spur, a small bony calcification on the calcans heel bone, in which case it is the underlying plantar fasciitis that produces the pain, and not the spur itself. The condition is responsible for the creation of the spur; the plantar fasciitis is not caused by the spur. Sometimes ball-of-foot pain is mistakenly assumed to be derived from plantar fasciitis. A dull pain or numbness in the metatarsal region of the foot could instead be metatarsalgia, also called capsulitis. Some current studies suggest that plantar fasciitis is not actually inflamed plantar fascia, but merely an inflamed flexor digitorum brevis muscle (FDB) belly. Ultrasound evidence illustrates fluid within the FDB muscle belly, not the plantar fascia.
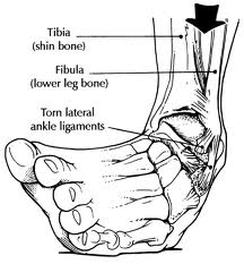 - ANKLE INVERSION SPRAIN
- ANKLE INVERSION SPRAIN
Inversion ankle sprains are the most common ankle sprain. An inversion sprain occurs when the foot rolls over onto the lateral side in an inward motion. This motion puts added stress on the ligaments of the outer ankle and often this stress proves to be too much and you will suffer a sprain. Pain is always felt on the outside of the ankle, simply because that is where the injury has occured. There are three ligaments, the anterior and posterior talofibular ligaments and the calcanefibular ligament, that make up the lateral collateral ligament (LCL) on the outside of the ankle; these are the ligament(s) that are stretched or torn during an inversion sprain.
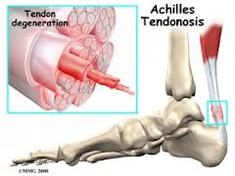 - ACHILLES TENDONOPATHY
- ACHILLES TENDONOPATHY
The painful Achilles tendon is a common presentation in orthopaedic and sports medicine clinics. Traditionally described as "Achilles tendonitis" it is now recognised that the inflammatory process is absent in most patients, and that this is a degenerative and overuse condition with attempted repair. Maffuli (1999) recommended the term “Achilles tendonopathy” to describe the clinical syndrome of pain, swelling and impaired performance in the Achilles tendon, reserving “tendinosis” for histopathological findings. Tendonopathy and tendinosis do not always co-exist.
 - MEDIAL TIBIAL STRESS SYNDROME (SHIN SPLINTS)
- MEDIAL TIBIAL STRESS SYNDROME (SHIN SPLINTS)
Medial tibial stress syndrome (MTSS), tibial periostisis or shin splints is a common injury that affects athletes who engage in running sports or physical activity. This condition is characterized by pain in the lower part of the leg between the knee and the ankle. MTSS injuries are caused by repeated trauma to the connective muscle tissue surrounding the tibia. Ignoring this injury may result in a more serious condition such as a stress fracture or breakage of the bones.
Causes and epidemiology Shin splints, known as medial tibial stress syndrome (MTSS), can usually be attributed to overloading the muscles of the lower extremities or to biomechanical irregularities. If an athlete begins running a lot after not running for a long period of time, it puts excess stress on the muscles, causing shin splints. Muscle imbalance, including weak core muscles, can cause lower-extremity injuries, and inflexibility and tightness of the gastrocnemius, soleus and plantar muscles (commonly the flexordigitorum longus) may contribute, as well. Increasing activity, intensity, and duration too quickly leads to shin splints because the tendons and muscles are unable to absorb the impact of the shock force as they become fatigued; also, the tibial bone-remodelling capabilities are overloaded. The pain associated with MTSS is caused from a disruption of Sharpey's fribres that connect the medial soleus fascia through the periosteum of the tibia where it inserts into the bone. With repetitive stress, the impact forces eccentrically fatigue the soleus and create repeated tibial bending or bowing; thus, contributing to MTSS. The impact is made worse by running uphill, downhill, on uneven terrain, or on hard surfaces. Improper footwear, including worn-out shoes can also contribute to shin splints. Risk factors for developing MTSS include:
Causes and epidemiology Shin splints, known as medial tibial stress syndrome (MTSS), can usually be attributed to overloading the muscles of the lower extremities or to biomechanical irregularities. If an athlete begins running a lot after not running for a long period of time, it puts excess stress on the muscles, causing shin splints. Muscle imbalance, including weak core muscles, can cause lower-extremity injuries, and inflexibility and tightness of the gastrocnemius, soleus and plantar muscles (commonly the flexordigitorum longus) may contribute, as well. Increasing activity, intensity, and duration too quickly leads to shin splints because the tendons and muscles are unable to absorb the impact of the shock force as they become fatigued; also, the tibial bone-remodelling capabilities are overloaded. The pain associated with MTSS is caused from a disruption of Sharpey's fribres that connect the medial soleus fascia through the periosteum of the tibia where it inserts into the bone. With repetitive stress, the impact forces eccentrically fatigue the soleus and create repeated tibial bending or bowing; thus, contributing to MTSS. The impact is made worse by running uphill, downhill, on uneven terrain, or on hard surfaces. Improper footwear, including worn-out shoes can also contribute to shin splints. Risk factors for developing MTSS include:
- Excessive pronation at subtalar joint
- Excessively tight calf muscles (which can cause excessive pronation)
- Engaging the medial shin muscle in excessive amounts of eccentric muscle activity
- Undertaking high-impact exercises on hard, noncompliant surfaces (ex: running on asphalt or concrete)
- Smoking and low fitness level
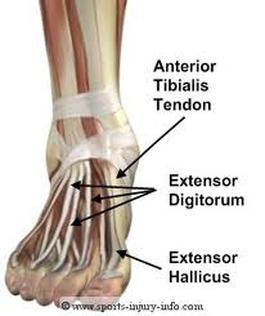 - ANTERIOR TIBIALIS TENDONOPATHY
- ANTERIOR TIBIALIS TENDONOPATHY
The tibialis anterior (i.e. front) muscle is situated at the front of the shin, connecting to important bones in the foot with the assistance of the tibialis anterior tendon. This muscle helps with dorsiflexion, and pressure is placed on the tendon whenever it is stretched or contracted. Repetitive high strain or too much force can cause damage to the tendon. This leads to degeneration and swelling in the area.
SYMPTOMS of Tibialis Anterior TendinopathyPain felt near the front of the foot or ankle, especially during or after a physical activity in which much strain is put on the tibialis anterior tendon. The pain may not be immediately felt, and it is common to experience the pain the next morning or after rest. It is likely to become sharper over time if physical activities involving this foot continue. Pressing on the area of the tendon itself may result in replicating the pain.
CAUSES of Tibialis Anterior TendinopathyActivities that place inordinate pressure on the tendon can result in the injury, either due to degeneration of the tendon over time or, rarely, because of a single incident in which the tendon is accidentally rubbed. This rarer cause is provoked by actions such as very tight tying of a bandage, guard, shoelaces or other material directly over the tendon. More commonly the tendinopathy is caused through repeated strain as caused in movements including quick walking or sprinting on hills or uneven ground (or excessively on flat surfaces), wearing very tight footwear, kicking a football, or kneeling. Many fast paced sports that require running and kicking can lead to the condition.
SYMPTOMS of Tibialis Anterior TendinopathyPain felt near the front of the foot or ankle, especially during or after a physical activity in which much strain is put on the tibialis anterior tendon. The pain may not be immediately felt, and it is common to experience the pain the next morning or after rest. It is likely to become sharper over time if physical activities involving this foot continue. Pressing on the area of the tendon itself may result in replicating the pain.
CAUSES of Tibialis Anterior TendinopathyActivities that place inordinate pressure on the tendon can result in the injury, either due to degeneration of the tendon over time or, rarely, because of a single incident in which the tendon is accidentally rubbed. This rarer cause is provoked by actions such as very tight tying of a bandage, guard, shoelaces or other material directly over the tendon. More commonly the tendinopathy is caused through repeated strain as caused in movements including quick walking or sprinting on hills or uneven ground (or excessively on flat surfaces), wearing very tight footwear, kicking a football, or kneeling. Many fast paced sports that require running and kicking can lead to the condition.
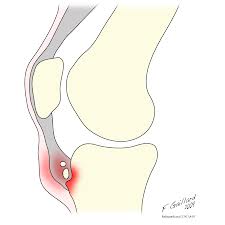
 - PATELLA TENDONITIS/KNEE PAIN
- PATELLA TENDONITIS/KNEE PAIN
Patellar tendonitis is the condition that occurs when the tendon becomes inflamed and irritated. This condition is most often seen in athletes who do repetitive jumping, the reason patellar tendonitis is often called "jumper's knee." Patellar tendonitis is most often seen in participants of sports including basketball and volleyball, although can also be seen in runners and other types of athletes. Patellar tendonosis is a chronic condition. Instead of the tendon becoming inflamed and irritated, the condition is more gradual in developing, and characterized by microscopic tears and thickening of the tendon. Patellar tendinosis causes similar symptoms, but the treatment of this condition is different from tendonitis. Partial patellar tendon tears, a finding sometimes described on an MRI, are usually characteristic of chronic patellar tendinosis. These tears are differentiated from a complete patellar tendon tear where the entire tendon is detached and requires surgical repair.
Symptoms of Patellar Tendon ConditionsPatellar tendonitis and tendinosis usually cause pain directly over the patellar tendon. The tendon is usually tender and swollen. Movement of the knee may causes a crunching sensation called cretitus directly over the swollen tendon. The other common symptom of patellar tendon problems is pain with activities, especially jumping or kneeling.X-ray tests are usually performed to confirm there is no problem with the bones around the knee. Occasionally, a calcium deposit may be seen, particularly in patients with a more chronic patellar tendinosis. An MRI may be helpful to look for symptoms of inflammation or partial tears within the tendon.
Symptoms of Patellar Tendon ConditionsPatellar tendonitis and tendinosis usually cause pain directly over the patellar tendon. The tendon is usually tender and swollen. Movement of the knee may causes a crunching sensation called cretitus directly over the swollen tendon. The other common symptom of patellar tendon problems is pain with activities, especially jumping or kneeling.X-ray tests are usually performed to confirm there is no problem with the bones around the knee. Occasionally, a calcium deposit may be seen, particularly in patients with a more chronic patellar tendinosis. An MRI may be helpful to look for symptoms of inflammation or partial tears within the tendon.
 - OSGOOD SCHLATTER
- OSGOOD SCHLATTER
Osgood–Schlatter disease or syndrome (also known as Apophysitis of the tibial tubercle, or knobby knees) is an irritation of the patellar ligament at the tibial tuberosity. It is characterized by painful lumps just below the knee and is most often seen in young adolescents. Risk factors may include overzealous conditioning (running and jumping), but adolescent bone growth is at the root of it. Osgood–Schlatter disease generally occurs in boys and girls aged 9–16 coinciding with periods of growth spurts. It occurs more frequently in boys than in girls, with reports of a male-to-female ratio ranging from 3:1 to as high as 7:1. It has been suggested that difference is related to a greater participation by boys in sports and risk activities than by girls. The condition is usually self-limiting and is caused by stress on the patellar tendon that attaches the quadriceps muscle at the front of the thigh to the tibial tuberosity. Following an adolescent growth spurt, repeated stress from contraction of the quadriceps is transmitted through the patellar tendon to the immature tibial tuberosity. This can cause multiple subacute avulsion fractures along with inflammation of the tendon, leading to excess bone growth in the tuberosity and producing a visible lump which can be very painful, especially when hit. Activities such as kneeling may also irritate the tendon. The syndrome may develop without trauma or other apparent cause; however, some studies report up to 50% of patients relate a history of precipitating trauma.
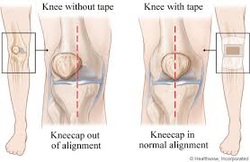 - PATELLA TRACKING SYNDROME
- PATELLA TRACKING SYNDROME
- Patella- the small bone in front of the knee, often called the kneecap. The patella allows the knee to work efficiently by gliding up and down the groove which allows the knee to bend and straighten. Femur- the biggest bone in the body, where the quadriceps tendon is attached. Tibia- the most weight bearing bone in the body, where the patellar tendon is attached Femoral Groove- the groove where the patella fits into. Is attached to the femur. The patella as the knee bends, is suppose to ride smoothly through the femoral groove. In patella tracking syndrome the patella is grinding against the groove causing it to move off to the left or right. By the petella doing this, it causes the cartilage to wear away. Patella Tracking Sydrome can also be called Patellofemoral Sydrome, or Chondromalacia. Some of the causes for patella tracking syndrome are: overusing the knee, having an abnormal Q-angle (the angle that measures the pull of the quadriceps muscle on the patella), and if you are a male or female. Females are more likely to get patella tracking syndrome, because of their more wide hips which makes their Q-angle bigger than a males
 - ILLIOTIBIAL BAND FRICTION SYNDROME
- ILLIOTIBIAL BAND FRICTION SYNDROME
Iliotibial band syndrome is one of the leading causes of lateral knee in runners. The Illiotibial band is a thick band of fascia on the lateral aspect of the knee, extending from the outside of the pelvis, over the hip and knee, and inserting just below the knee. The band is crucial to stabilizing the knee during running, as it moves from behind the femur to the front of the femur during activity. The continual rubbing of the band over the lateral femoral epicondyle, combined with the repeated flexion and extension of the knee during running may cause the area to become inflamed. Symptoms ITBS symptoms range from a stinging sensation just above the knee joint, to swelling or thickening of the tissue in the area where the band moves over the femur. The stinging sensation just above the knee joint is felt on the outside of the knee or along the entire length of the illiotibial band Pain may not occur immediately during activity, but may intensify over time. Pain is most commonly felt when the foot strikes the ground, and pain might persist after activity. Pain may also be present above and below the knee, where the ITB attaches to the tibia. Causes ITBS can result from one or more of the following: training habits, anatomical abnormalities, or muscular imbalances:
Training habits:
Training habits:
- Consistently running on a banked surface, which causes the downhill leg to bend slightly inward, causing extreme stretching of the band against the femur (such as the shoulder of a road or an indoor track). - Inadequate warm-up or cool-down - Excessive up-hill and down-hill running - Positioning the feet "toed-in" to an excessive angle when cycling - Running up and down stairs - Hiking long distances - Rowing - Breaststroke - Treading Water - Egg Beater (Water Polo) - Abnormalities in leg/feet anatomy: - high or low arches - Supination of the foot - Excessive lower leg rotation due to over-pronation - Excessive foot strike force - Uneven leg length - Bowlegs or tightness about the iliotibial band. - Muscle imbalance: - Weak hip abductor muscles - Weak/non-firing multifidus muscle
 - MEDIAL KNEE PAIN/SPRAIN (MCL SPRAIN)
- MEDIAL KNEE PAIN/SPRAIN (MCL SPRAIN)
Medial knee pain is pain that occurs on the inner side of the knee and can be due to a number of problems.
It may come on gradually over time or may develop suddenly after a knee injury. It may be a general inner knee pain, movement may be restricted or there may be a sharp pain.
It is very common to get pain on the medial side of the knee, because muscle weakness and/or tightness (which is very common) can subtly change the way the knee moves. This causes more force to go through the inner side of the joint, rather than distributing weight evenly through the whole joint, which results in damage to the inner side of the knee and therefore medial knee pain.
Here you will find a summary of the three most common causes of medial knee pain. Click on the links to find out more about each condition including symptoms and treatment options for each. If you want more help working out what is wrong with your knee, visit the knee pain diagnosis section.
It may come on gradually over time or may develop suddenly after a knee injury. It may be a general inner knee pain, movement may be restricted or there may be a sharp pain.
It is very common to get pain on the medial side of the knee, because muscle weakness and/or tightness (which is very common) can subtly change the way the knee moves. This causes more force to go through the inner side of the joint, rather than distributing weight evenly through the whole joint, which results in damage to the inner side of the knee and therefore medial knee pain.
Here you will find a summary of the three most common causes of medial knee pain. Click on the links to find out more about each condition including symptoms and treatment options for each. If you want more help working out what is wrong with your knee, visit the knee pain diagnosis section.
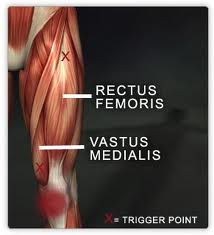 - RECTUS FEMORIS STRAIN
- RECTUS FEMORIS STRAIN
The rectus femoris is one of the quadriceps muscles of the thigh. It crosses two joints – the hip and knee. It is commonly injured as the tendon at the front of the hip or in the muscle belly of the thigh. This injury is what many people refer to as a “hip flexor strain.” It is a common injury in sports such as soccer and football. Usually it involves a forceful movement such as immediately starting to sprint or forcefully kicking a ball, especially when the athlete’s foot strikes another player while trying to kick.
These injuries are almost always acute ones. The football player or soccer player will notice immediately that an injury has occurred. With a rectus femoris tendon strain, the athlete will localize the pain to the front of the hip. A sports medicine physician examining the player might notice a defect in this area if a full tear is present, but a full tear is unusual. More frequently, the physician will notice pain or weakness with resisted hip flexion or resisted knee extension. He or she might order x-rays to determine if the athlete pulled a small piece of bone off one of the bones in the hip, as you can occasionally see in young athletes who are not done growing. In high-level athletes especially, the physician might order an MRI of the hip. The MRI will help to confirm which tendon is involved. It can also give a better idea of the extent of injury and how long it might take the athlete to recover and return to sports.
These injuries are almost always acute ones. The football player or soccer player will notice immediately that an injury has occurred. With a rectus femoris tendon strain, the athlete will localize the pain to the front of the hip. A sports medicine physician examining the player might notice a defect in this area if a full tear is present, but a full tear is unusual. More frequently, the physician will notice pain or weakness with resisted hip flexion or resisted knee extension. He or she might order x-rays to determine if the athlete pulled a small piece of bone off one of the bones in the hip, as you can occasionally see in young athletes who are not done growing. In high-level athletes especially, the physician might order an MRI of the hip. The MRI will help to confirm which tendon is involved. It can also give a better idea of the extent of injury and how long it might take the athlete to recover and return to sports.

A hamstring strain is a common injury involving a tear in one or more of the hamstring muscles. A pulled hamstring can range from mild to very severe involving a complete tear of the muscle. One of the most obvious symptoms of a hamstring strain is a sudden sharp pain at the back of the leg during exercise, most probably during sprinting or high speed movements. Depending on how bad the injury is the athlete will usually have to stop immediately and further participation in training or sport difficult or impossible. Often the athlete will try to play on with a pulled hamstring but this is one injury where it just isn't possible. The hamstring muscle group consists of three separate muscles; the semitendinosus, semimembranosus and biceps femoris. During sprinting the hamstring muscles work extremely hard to decelerate the tibia or shin bone as it swings out. It is in this phase just before the foot strikes the ground that the hamstrings become injured as the muscles are working hardest at the same time as approaching their maximum length. A pulled hamstring rarely manifests as a result of contact. If you have taken an impact to the back of the leg it should be treated as a contusion until found to be otherwise. A strained or pulled hamstring as it is sometimes called is a tear in one or more of the hamstring muscles. Problems with the lower back and pelvis may increase the likelihood of suffering a hamstrings strain and should always be considered, particularly for recurrent hamstring injuries. Pulled hamstrings are graded 1, 2 or 3 depending on severity. Grade 1 consists of minor tears within the muscle. A grade 2 is a partial tear in the muscle and grade 3 is a severe or complete rupture of the muscle. Grade 1 Hamstring strain With a grade 1 hamstring strain the athlete may have tightness in back of the thigh but will be able to walk normally. They will be aware of some discomfort and unable to operate at full speed. There will be little swelling and trying to bend the knee against resistance is unlikely to reproduce much pain. Grade 2 Hamstring strain With a grade 2 hamstring strain the athletes gait will be affected and they will most likely be limping. Sudden twinges of pain during activity will be present. They may notice some swelling and pain will be reproduced when pressing in on the hamstring muscle as well as trying to bend the knee against resistance. Grade 3 Hamstring strain A grade 3 hamstring strain is a severe injury involving a tear to half or all of the muscle. The athlete may need crutches to walk and will feel severe pain and weakness in the muscle. Swelling will be noticeable immediately and bruising will usually appear within 24 hours.
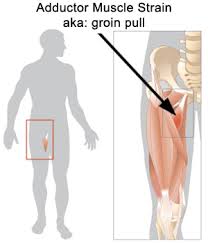 - ADDUCTORS OR GROIN STRAIN
- ADDUCTORS OR GROIN STRAIN
A groin strain is a tear or rupture to any one of the five adductor muscles. We explain the symptoms, diagnosis, treatment and rehabilitation including sports massage and exercises. Groin strain symptomsSymptoms of an acute groin strain typically include a sudden sharp pain in the groin area, either in the belly of the muscle or higher. The athlete may or may not be able to play on depending on how bad it is. There may also be rapid swelling followed by bruising. Groin strains are graded 1, 2 or 3 depending on the extent of the injury.
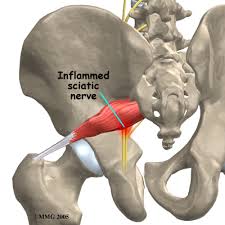 - PIRIFORMIS
- PIRIFORMIS
No one really knows exactly what causes piriformis syndrome, or if it really exists. Some physicians believe that piriformis syndrome is the name given to hip/buttock pain that cannot be otherwise diagnosed. Others believe that piriformis syndrome is a very real cause of pain and disability.What is the piriformis muscle?
The piriformis is a muscle that travels behind the hip joint. The piriformis muscle is small compared to other muscles around the hip and thigh, and it aids in external rotation (turning out) of the hip joint. The piriformis muscle and its tendon have an intimate relationship to the sciatic nerve--the largest nerve in the body--which supplies the lower extremities with motor and sensory function. The piriformis tendon and sciatic nerve cross each other behind the hip joint, in the deep buttock. Both structures are about one centimeter in diameter.
The piriformis is a muscle that travels behind the hip joint. The piriformis muscle is small compared to other muscles around the hip and thigh, and it aids in external rotation (turning out) of the hip joint. The piriformis muscle and its tendon have an intimate relationship to the sciatic nerve--the largest nerve in the body--which supplies the lower extremities with motor and sensory function. The piriformis tendon and sciatic nerve cross each other behind the hip joint, in the deep buttock. Both structures are about one centimeter in diameter.
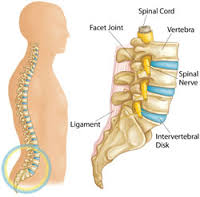 - LUMBAR SPINE
- LUMBAR SPINE
Physicians use a code to number each of the 24 vertebrae in the spine. The low back officially begins with the lumbar region of the spine directly below the cervical and thoracic regions and directly above the sacrum. The lumbar vertebrae, L1-L5, are most frequently involved in back pain because these vertebrae carry the most amount of body weight and are subject to the largest forces and stresses along the spine. The true spinal cord ends at approximately the L1 level, where it divides into many different nerve roots that travel to the lower body and legs. This collection of nerve roots is called the "cauda equina," which means horse's tail and describes the continuation of the nerve roots at the end of the spinal cord.
Vertebrae: The vertebral body is a thin ring of dense cortical bone. The vertebral body is shaped like an hourglass, thinner in the center with thicker ends. Outer cortical bone extends above and below the superior and inferior ends of the vertebrae to form rims. The superior and inferior endplates are contained within these rims of bone.
Vertebrae: The vertebral body is a thin ring of dense cortical bone. The vertebral body is shaped like an hourglass, thinner in the center with thicker ends. Outer cortical bone extends above and below the superior and inferior ends of the vertebrae to form rims. The superior and inferior endplates are contained within these rims of bone.
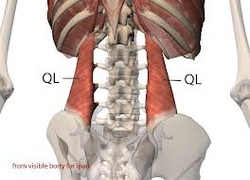 - QUADRATUS LUMBORUM
- QUADRATUS LUMBORUM
After years of experience, I have come to believe there is nothing more complex to differentiate, diagnose, and treat than low back pain. Western orthopedic evaluation does a great job when there is a disc herniation with a protrusion or fragment lodged on a spinal nerve root. Anything else, in my opinion, is either art or guesswork. I see many patients who have been to numerous physicians, each diagnosing a different cause of pain. Unfortunately, TCM diagnosis is no better. I gave up on treatment based upon the meridian (jing-luo) perspective years ago when Bladder meridian points such as Bl 23, Bl 25, Bl 40 and Bl 60 gave my patients inadequate results. And from an internal organ viewpoint, I have never found treating the Kidney, which controls the lower back, to be clinically reliable. Back pain is a complicated and comprehensive condition, and it is not the purpose of this article to articulate on the subject. However, I would like to discuss how acupuncture treatment to the quadratus lumborum (QL) muscle is important to consider in any treatment plan for lumbar, sacral, and gluteal pain. While this muscle might not be the entire cause of pain - other points, treatments, and techniques may be necessary - the simple techniques that follow benefit many patients and may serve as an important protocol for acupuncture treatment. The following is a brief summary of the pain due to quadratus lumborum dysfunction:
Common patient complaints Acute back pain and spasm - Patient may report the spine feels "locked up" - Pain is often one-sided - Pain may radiate towards the gluteal region
Common patient complaints Acute back pain and spasm - Patient may report the spine feels "locked up" - Pain is often one-sided - Pain may radiate towards the gluteal region
- Some patients may have chronic QL dysfunction.
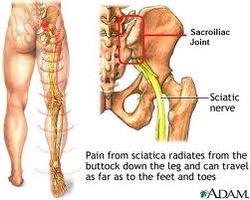 - SI JOINT INFLAMMATION
- SI JOINT INFLAMMATION
The sacroiliac joint (abbreviated 'SI joint') is a firm, thin joint that is at the junction of the spine and the pelvis. Most often when we think of joints, we think of knees, hips, and shoulders--joints that are made to undergo motion. The sacroiliac joint does not move much, but it is critical to transferring the load of your upper body to your lower body.SI joint pain is most often joint inflammation as a result of repetitive activity or overuse. People often refer to SI joint inflammation as sacroilitis. Other causes of SI joint pain include arthritis of the SI joint, infection of the SI joint, or ligament sprains of the ligaments that surround the SI joint.
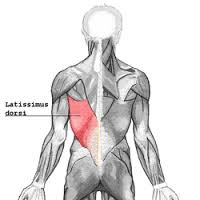 - LATISSIMUS DORSI
- LATISSIMUS DORSI
The latissimus dorsi meaning 'broadest [muscle] of the back' (Latin latus meaning 'broad', latissimusmeaning 'broadest' and dorsum meaning the back), is the larger, flat, dorso-lateral muscle on the trunk, posterior to the arm, and partly covered by the Trapezius on its median dorsal region. Latissimi dorsi are commonly known as "lats", especially among bodybuilders.
The latissimus dorsi is responsible for extension, adduction, transverse extension also known as horizontal abduction, flexion from an extended position, and (medial) internal rotation of the shoulder joint. It also has a synergistic role in extension and lateral flexion of the lumbar spine.
Due to bypassing the scapulothoracic joints and attaching directly to the spine, the actions the latissimi dorsi have on moving the arms can also influence the movement of the scapulae, such as their downward rotation during a pull up.
The latissimus dorsi is responsible for extension, adduction, transverse extension also known as horizontal abduction, flexion from an extended position, and (medial) internal rotation of the shoulder joint. It also has a synergistic role in extension and lateral flexion of the lumbar spine.
Due to bypassing the scapulothoracic joints and attaching directly to the spine, the actions the latissimi dorsi have on moving the arms can also influence the movement of the scapulae, such as their downward rotation during a pull up.
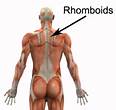 - RHOMBOIDS
- RHOMBOIDS
The rhomboid muscles, often simply called the rhomboids, are rhomboid rhumbus-shaped muscles associated with the scapula and are chiefly responsible for its retraction. It is supplied by Dorsal Scapular nerve. There are two rhomboid muscles:
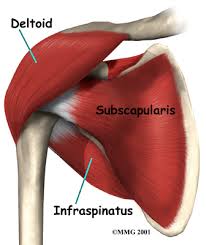 - DELTOID
- DELTOID
In human anatomy, the deltoid muscle is the muscle forming the rounded contour of the shoulder. Anatomically, it appears to be made up of three distinct sets of fibers though electromyography suggests that it consists of at least seven groups that can be independently coordinated by the central nervous system.
It was previously called the deltoideus and the name is still used by some anatomists. It is called so because it is in the shape of the Greek letter Delta (triangle). It is also known as the common shoulder muscle, particularly in lower animals (e.g., in domestic cats). Deltoid is also further shortened in slang as "delt". The plural forms of all three incarnations are deltoidei, deltoids and delts.
It was previously called the deltoideus and the name is still used by some anatomists. It is called so because it is in the shape of the Greek letter Delta (triangle). It is also known as the common shoulder muscle, particularly in lower animals (e.g., in domestic cats). Deltoid is also further shortened in slang as "delt". The plural forms of all three incarnations are deltoidei, deltoids and delts.
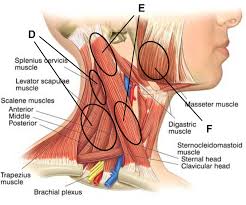 -SCELENES
-SCELENES
The scalene muscles (from Greek σκαληνός, or skalenos, meaning uneven as the pairs are all of differing length) are a group of three pairs of muscles in the lateral neck, namely thescalenus anterior, Scalenus Medius, and scalenus posterior. They are innervated by the fourth, fifth, and sixth cervical spinal nervewsspinal nerves (C4-C6).
A fourth muscle, the scalenus minimus (Sibson's muscle), is sometimes present behind the lower portion of the scalenus anterior
A fourth muscle, the scalenus minimus (Sibson's muscle), is sometimes present behind the lower portion of the scalenus anterior
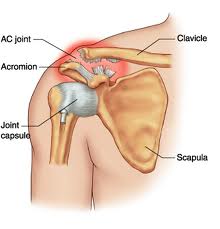 - A/C JOINT SPRAIN
- A/C JOINT SPRAIN
An AC joint sprain is a relatively common sporting injury affecting the shoulder and is characterized by tearing of the connective tissue and ligaments of the Acromio-Clavicular joint. The shoulder blade gives rise to a bony prominence known as the acromion. The acromion attaches to the collar bone (clavicle) via strong ligaments and connective tissue. This joint is known as the AC joint and is situated at the point of the shoulder (figure 1). The AC joint is responsible for connecting the shoulder blade with the clavicle and allows for some shoulder movement. During certain activities, stretching forces are placed on the AC joint. When these forces are excessive and beyond what the AC joint can withstand, tearing of the ligaments and connective tissue of the AC joint may occur. This condition is known as an AC joint sprain.An AC joint sprain can range from a small sprain resulting in minimal pain and allowing ongoing activity, to a severe sprain resulting in significant pain, deformity and disability. Causes of an AC joint sprainAn AC joint sprain typically occurs due to a specific incident such as a direct blow to the point of the shoulder. This commonly occurs in contact sports due to a collision with another player or following a fall onto the point of the shoulder. Signs and Symptoms of an AC joint sprainPatients with this condition typically experience a sudden onset of pain on the top of the shoulder at the time of injury. Pain may increase with activities involving lying on the affected side, moving the arm across the body, overhead activity or performing heavy lifting, pushing or pulling movements with the affected arm. In minor cases of an AC joint sprain, patients may be able to continue activity only to experience an increase in pain, swelling and stiffness in the shoulder after activity with rest (particularly first thing in the morning). In more severe cases, pain may prevent the patient from continuing activity and cause them to cradle the arm. Patients may also experience a rapid onset of swelling and may notice a 'step' deformity or bump in their shoulder with the tip of their collar bone sticking up. This occurs due to tearing of the connective tissue holding the AC joint together and the accumulation of swelling and bleeding around the joint.
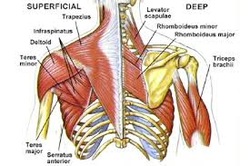 - LEVATOR SCAPULA/UPPER TRAPEZIUZ
- LEVATOR SCAPULA/UPPER TRAPEZIUZ
In human anatomy, the levator scapulae (/ˌlɨˈveɪtər ˈskæpjʉliː/) is a skeletal muscle situated at the back and side of the neck. As the name suggests, its main function is to lift the scapula.
 - NECK & CERVICAL PAIN
- NECK & CERVICAL PAIN
Neck pain (or cervicalgia) is a common problem, with two-thirds of the population having neck pain at some point in their lives. Neck pain, although felt in the neck, can be caused by numerous other spinal problems. Neck pain may arise due to muscular tightness in both the neck and upper back, or pinching of the nerves emanating from the cervoca; vertibrea. Joint disruption in the neck creates pain, as does joint disruption in the upper back.
The head is supported by the lower neck and upper back, and it is these areas that commonly cause neck pain. The top three joints in the neck allow for most movement of the neck and head. The lower joints in the neck and those of the upper back create a supportive structure for the head to sit on. If this support system is affected adversely, then the muscles in the area will tighten, leading to neck pain.
The head is supported by the lower neck and upper back, and it is these areas that commonly cause neck pain. The top three joints in the neck allow for most movement of the neck and head. The lower joints in the neck and those of the upper back create a supportive structure for the head to sit on. If this support system is affected adversely, then the muscles in the area will tighten, leading to neck pain.
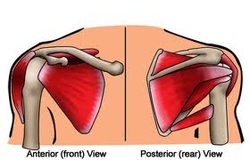 - ROTATOR CUFF-SUPRASPINATUS & INFRASPINATUS
- ROTATOR CUFF-SUPRASPINATUS & INFRASPINATUS
A rotator cuff tear is a tear of one or more of the tendons of the four rotator cuff muscles. A rotator cuff injury can include any type of irritation or damage to the rotator cuff muscles or tendons. Rotator cuff tears are among the most common conditions affecting the shoulder. The tendons of the rotator cuff, not the muscles, are most commonly involved and of the four, the supraspinatus most frequently, as it passes below the acromion. Such a tear usually occurs at its point of insertion onto the humeral head at the greater tubercle. The cuff is responsible for stabilizing the glenohumeral joint and rotating the humerous outward (external rotation). When shoulder trauma occurs, these functions can be compromised. Because individuals are highly dependent on the shoulder for many activities, overuse of the muscles can lead to tears, with the vast majority again occurring in the supraspinatus tendon. The supraspinatus (plural supraspinati, from Latin supraspinatus) is a relatively small muscle of the upper back that runs from the supraspinatous fossa superior of the scapula (shoulder blade) to the greater tubercle of the humerus. It is one of the four rotator cuff muscles and also abducts the arm at the shoulder. The spine of the scapula separates the supraspinatus muscle from the infraspinatus muscle, which originates below the spine. In human anatomy, the infraspinatus muscle is a thick triangular muscle, which occupies the chief part of the infraspinatous fossa.[1] As one of the four muscles of the rotator cuff, the main function of the infraspinatus is to externally rotate the humerus and stabilize the shoulder joint.
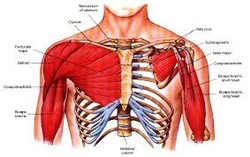 - PECTORALIS MINOR/MAJOR
- PECTORALIS MINOR/MAJOR
From the surface of pectoralis major, some superficial fibers arise from the fascia of the clavicular head and are inserted into the fascia of the deltoid muscle. M. Sternalis (in 3-5% of individuals) is a fleshy band of longitudinal fibers, often bilateral, of varying length and width, located close to and, generally, parallel to the sternum. When typical, it arises from the sheath of the rectus abdominis, fascia of the external oblique, pectoralis major, or costal cartilages (3-7) and ends above in fascia, upper costal cartilages, or manubrium, or may be joined to the the sternal or medial head of sternocleidomastoideus. The muscle may exhibit tendinous inscriptions. It is considered by some authors to be a vestige of the panniculus carnosus. In a study of 1000 cadavers (438 females and 562 males), sternalis was found more frequently in females (8.7%) than males (6.4). Its reported incidence in the white population is about 4.-7%, the black population about 8.4%, and in the Asian population about 11.5%. (see also m. supracostalis).
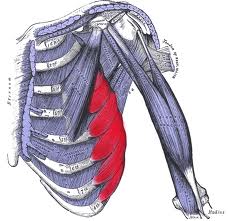 - SERRATUS ANTERIOR PAIN
- SERRATUS ANTERIOR PAIN
Because the serratus anterior is largely hidden from view underneath the shoulder blade, it is remarkably easy for both patients and clinicians to forget about this vital muscle. It originates from the underside of the shoulder blade near the inner edge and has a broad attachment to the ribs. It gets its name from the way that it is serrated, like a knife blade, as it attaches into the ribs, and is anterior (forward to) the shoulder blade. Even though the serratus anterior is not visible on most people’s bodies, it is normally a very strong and fairly large muscle. And here is where the confusion REALLY sets in. The serratus anterior has historically been though of as performing two primary functions. The first is to hold inner edge of the shoulder blade against the ribs, preventing ‘winging’ of the shoulder blade,
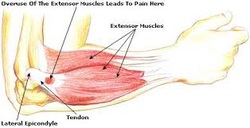 - TENNIS ELBOW
- TENNIS ELBOW
Tennis elbow or lateral epicondylitis is a condition in which the outer part of the elbow becomes sore and tender. It is commonly caused by non-inflammatory, chronic degenerative changes in the tendon that attaches the forearm muscle extensor carpi radialis brevis to the elbow. It is most prevalent in middle age. Most of the names for this disease are misnomers: tennis elbow is a misnomer because most people that get this disease don't play tennis and lateral epicondylitis is a misnomer because the pathophysiology does not involve inflammation (it is an -osis, not an itis). The disease is idiopathic, benign, and self-limiting. Tennis ElbowClassification and external resources.
 - GOLFERS ELBOW
- GOLFERS ELBOW
Golfer's elbow, or medial epicondylitis, is an inflammatory condition of themedial epicondyle of the elbow. It is in some ways similar to tennis elbow. The anterior forearm contains several muscles that are involved with flexing the fingers and thumb, and flexing and pronating the wrist. The tendons of these muscle come together in a common tendinous sheath, which is inserted into the medial epicondyle of the humerus at the elbow joint. In response to minor injury, or sometimes for no obvious reason at all, this point of insertion becomes inflamed.
The condition is called Golfer's Elbow because in making a golf swing this tendon is stressed, especially if a non-overlapping (baseball style) grip is used; many people, however, who develop the condition have never handled a golf club. It is also sometimes called Pitcher's Elbow due to the same tendon being stressed by the throwing of objects such as a baseball, but this usage is much less frequent. Other names are Climber's Elbow andLittle League Elbow: All of the flexors of the fingers insert at the medial epicondyle, making this the most common elbow injury for rock climbers, whose sport is very grip intensive. Epicondylitis is much more common on the lateral side of the elbow, rather than the medial side. In most cases, its onset is gradual and symptoms often persist for weeks before patients seek care. In golfer's elbow, pain at the medial epicondyle is aggravated by resisted wrist flexion and pronation, which is used to aid diagnosis. On the other hand, tennis elbow is indicated by the presence of lateral epicondylar pain precipitated by resisted wrist extension. Although the condition is poorly understood at a cellular and molecular level, there are hypotheses that point to apoptosis and autophagic cell death as causes of chronic lateral epicondylitis. The cell death may decrease the muscle density and cause a snowball effect in muscle weakness - this susceptibility can compromise a muscle's ability to maintain its integrity. So athletes, like pitchers, must work on preventing this cell death via flexibility training and other preventative measures.
The condition is called Golfer's Elbow because in making a golf swing this tendon is stressed, especially if a non-overlapping (baseball style) grip is used; many people, however, who develop the condition have never handled a golf club. It is also sometimes called Pitcher's Elbow due to the same tendon being stressed by the throwing of objects such as a baseball, but this usage is much less frequent. Other names are Climber's Elbow andLittle League Elbow: All of the flexors of the fingers insert at the medial epicondyle, making this the most common elbow injury for rock climbers, whose sport is very grip intensive. Epicondylitis is much more common on the lateral side of the elbow, rather than the medial side. In most cases, its onset is gradual and symptoms often persist for weeks before patients seek care. In golfer's elbow, pain at the medial epicondyle is aggravated by resisted wrist flexion and pronation, which is used to aid diagnosis. On the other hand, tennis elbow is indicated by the presence of lateral epicondylar pain precipitated by resisted wrist extension. Although the condition is poorly understood at a cellular and molecular level, there are hypotheses that point to apoptosis and autophagic cell death as causes of chronic lateral epicondylitis. The cell death may decrease the muscle density and cause a snowball effect in muscle weakness - this susceptibility can compromise a muscle's ability to maintain its integrity. So athletes, like pitchers, must work on preventing this cell death via flexibility training and other preventative measures.
 CARPAL TUNNEL PAIN
CARPAL TUNNEL PAIN
Carpal tunnel syndrome occurs when the median nerve, which runs from the forearm into the palm of the hand, becomes pressed or squeezed at the wrist. The median nerve controls sensations to the palm side of the thumb and fingers (although not the little finger), as well as impulses to some small muscles in the hand that allow the fingers and thumb to move. The carpal tunnel - a narrow, rigid passageway of ligament and bones at the base of the hand - houses the median nerve and tendons. Sometimes, thickening from irritated tendons or other swelling narrows the tunnel and causes the median nerve to be compressed. The result may be pain, weakness, or numbness in the hand and wrist, radiating up the arm. Although painful sensations may indicate other conditions, carpal tunnel syndrome is the most common and widely known of the entrapment neuropathies in which the body's peripheral nerves are compressed or traumatized. What are the symptoms of carpal tunnel syndrome? Symptoms usually start gradually, with frequent burning, tingling, or itching numbness in the palm of the hand and the fingers, especially the thumb and the index and middle fingers. Some carpal tunnel sufferers say their fingers feel useless and swollen, even though little or no swelling is apparent. The symptoms often first appear in one or both hands during the night, since many people sleep with flexed wrists. A person with carpal tunnel syndrome may wake up feeling the need to "shake out" the hand or wrist. As symptoms worsen, people might feel tingling during the day. Decreased grip strength may make it difficult to form a fist, grasp small objects, or perform other manual tasks. In chronic and/or untreated cases, the muscles at the base of the thumb may waste away. Some people are unable to tell between hot and cold by touch. What are the causes of carpal tunnel syndrome? Carpal tunnel syndrome is often the result of a combination of factors that increase pressure on the median nerve and tendons in the carpal tunnel, rather than a problem with the nerve itself. Most likely the disorder is due to a congenital predisposition - the carpal tunnel is simply smaller in some people than in others. Other contributing factors include trauma or injury to the wrist that cause swelling, such as sprain or fracture; overactivity of the pituitary gland; hypothyroidism; rheumatoid arthritis; mechanical problems in the wrist joint; work stress; repeated use of vibrating hand tools; fluid retention during pregnancy or menopause; or the development of a cyst or tumor in the canal. In some cases no cause can be identified. There is little clinical data to prove whether repetitive and forceful movements of the hand and wrist during work or leisure activities can cause carpal tunnel syndrome. Other disorders such as bursitis and tendonitis have been associated with repeated motions performed in the course of normal work or other activities.. Writer's cramp may also be brought on by repetitive activity.

A biceps strain occurs when the muscle, which is located between your elbow and shoulder on the front of your upper arm, is overstretched, causing some or all of the muscle fibers to tear. The rehabilitation process is lengthy, depending on the severity of the injury, and generally entails a period of rest followed by physical therapy to restore range of motion and strength to the affected area. Consult your doctor and a physical therapist to develop a comprehensive treatment plan.